
How should offices and other indoor spaces be ventilated to keep people safe from COVID-19? A recent paper by Rajesh Bhagat, Paul Linden and Stuart Dalziel of the Department of Applied Mathematics (DAMTP), and Megan Davies Wykes of the Department of Engineering, has some answers - and shows that wearing masks does make a difference.
"As winter approaches in the northern hemisphere and people start spending more time inside, understanding the role of ventilation is critical to estimating the risk of contracting the virus and helping slow its spread," says Linden, Director or Research and G.I. Taylor Professor Emeritus of Fluid Mechanics at DAMTP, who has studied the ventilation of buildings since 1990 and is a pioneer in the area. Previously Linden's aim was to make those buildings energy efficient and comfortable for their occupants, but in the light of the pandemic his work has taken on a new dimension. Since April he has been contributing to the Royal Society's Rapid Assistance in Modelling the Pandemic (RAMP) taskforce, which unites scientists and mathematicians in the effort to fight the pandemic.
Mixing or layering?
Evidence suggests that the virus which causes COVID-19 is transmitted mostly through larger droplets and smaller aerosols, which we expel when we breathe, talk, cough or laugh. These are hard to monitor, but the work of Linden and his colleagues confirms earlier research which suggests that CO2 can be used as a proxy. "Small respiratory aerosols containing the virus are transported along with the carbon dioxide produced by breathing, and are carried around a room by ventilation flows," explains Linden. "Insufficient ventilation can lead to high carbon dioxide concentration, which in turn could increase the risk of exposure to the virus."
Many modern indoor spaces, such as offices, hospitals, or restaurants, use some sort of ventilation system. The way the ventilation is achieved varies — you could use either natural ventilation driven by wind and heat, or mechanical systems — but there are two main modes of operation. Mixing ventilation aims to keep the air in a space well-mixed and displacement ventilation creates a cooler lower zone and a warmer upper zone, with warm air being extracted through the top part of the room and cooler air supplied through vents near the floor.
When it comes to transmission of COVID-19, it seems obvious that mixing up the air isn't the way you'd want to go, and the work of Linden and his team broadly supports this idea. "[Mixing ventilation] is intended to keep everything airborne and stirred around, and if it works properly then that's what mixing ventilation does," Linden explains. "I think essentially that's not a good idea and there are better strategies you can adapt." Displacement ventilation appears to be such a strategy: the warm and potentially dangerous air we exhale will rise to the ceiling, where it can be extracted.
What Linden and his colleagues also showed, however, is that things aren't quite as simple as they might first seem. Ventilation systems aren't the only things that cause significant air flows in a room. Other factors — people moving around, the opening and closing of doors, and heat emanating from people's bodies or appliances — can also cause the air to move in ways you can't just ignore. This means that even with displacement ventilation you can run into trouble: when there are various heat sources in a room, exhaled breath can get trapped below the warm ceiling layer and breathed in again by others.
Such insights can often be gained through mathematical models of airflows, but the exact behaviour of people's exhaled breath and its role in disease transmission is extremely difficult to predict. So Linden and his colleagues headed to the lab. They did this in the middle of the spring lockdown, when the fluid dynamics laboratory was the only part of the Centre for Mathematical Sciences that was open, and only to a select few.
Breathing, talking, laughing
Even when a person is sitting still and holding their breath, their body heat produces a plume of warm air that rises to the ceiling. When the person starts breathing, or opens their mouth to talk, sing, cough or laugh, their exhaled breath produces a second plume. In terms of transmission, it's best for this second plume to be entrained by the main body plume to be carried to the ceiling with it.
Air is invisible, of course, but Linden and his team used an imaging technique that allows you to track warm air. "You can see the change in temperature and density when someone breathes out warm air – it refracts the light and you can measure it,"explains Bhagat.
The images the team produced are shown below. In the left hand image the person is sitting quietly breathing through their nose, in the middle one he is speaking at a normal volume, and in the right one he is laughing. In each image, you can also see the body plume rising up gently — and in each of the three cases, you can see that the exhaled plume isn't absorbed by the body plume.
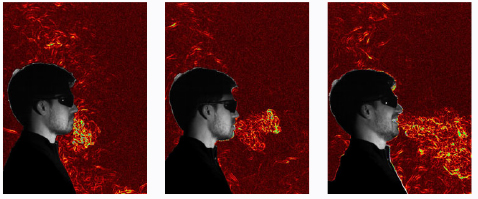
Image from Bhagat, R., Davies Wykes, M., Dalziel, S., & Linden, P. (2020). Effects of ventilation on the indoor spread of COVID-19. Journal of Fluid Mechanics, 903, F1.
This is in contrast to the images you get when the person is wearing a mask, shown below. "One thing we could clearly see is that one of the ways that masks work is by stopping the breath's momentum," said Linden.
"While pretty much all masks will have a certain amount of leakage through the top and sides, it doesn't matter that much, because slowing the momentum of any exhaled contaminants reduces the chance of any direct exchange of aerosols and droplets as the breath remains in the body's thermal plume and is carried upwards towards the ceiling. Additionally, masks stop larger droplets, and a three-layered mask decreases the amount of those contaminants that are recirculated through the room by ventilation."
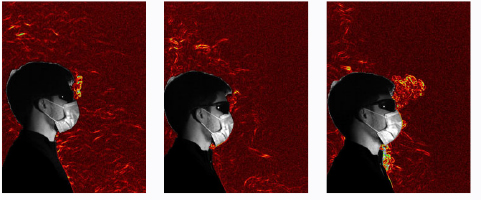
Image from Bhagat, R., Davies Wykes, M., Dalziel, S., & Linden, P. (2020). Effects of ventilation on the indoor spread of COVID-19. Journal of Fluid Mechanics, 903, F1.
A warning system
Linden and his colleagues stress that there's still more work to do on ventilation and COVID-19. For example, it would be good to know more about what happens to people's body plumes and exhaled breath as they move around a room. But the work done so far already carries an important message. Displacement ventilation systems, when properly set up, appear to be the better option, and face coverings are beneficial.
The research also suggests another interesting possibility. Since virus-laden aerosols behave like the CO2 we breathe out, the CO2 level in a room could provide a warning system. It can quite easily be measured, and when it's high, the risk of airborne infection is high too. "What we have in mind is something like a traffic light system," explains Linden. "But what we are not clear about yet is [which CO2 thresholds should mark the boundaries between green, amber and red]. So that's an area that still needs discussion."
For those of us without ventilation systems or ways of measuring CO2, the message is simple. When there are several people in a room, open the windows, keep your distance, and wear your masks.
The paper "Effects of ventilation on the indoor spread of COVID-19" by Rajesh K. Bhagat, M. S. Davies Wykes, Stuart B. Dalziel, and P. F. Linden is published in the Journal of Fluid Mechanics, 903, F1.
Some of the quotes in this article are taken from Many ventilation systems may increase risk of COVID-19 exposure, study suggests, reproduced under a Creative Commons Attribution 4.0 International License.
